An Oxford University led study, working with the University of Cape Town in South Africa, has found that text message reminders can help reduce people’s blood pressure.
The study, of over 1300 adults with high blood pressure in the Cape Town area, compared text message reminders and interactive text messaging to a control group receiving standard care. The results appear online in the American Heart Association journal Circulation.
Professor Andrew Farmer, from Oxford’s Department of Primary Health Care Sciences explained: 'High blood pressure is a common condition that can be managed successfully with tablets. Yet, even in health systems where that medication is freely available, people can struggle to keep taking the tablets regularly.
'Two common issues are not turning up to collect medicine – so running out – or forgetting to take tablets. We knew that text messages had worked to support people with HIV/Aids to stick to their treatment and improve their health as a result. We wanted to see whether the messages could work for blood pressure treatment in a deprived community.'
In the area of Cape Town chosen for the trial, around a third of families live in shacks and almost two thirds have a monthly income less than 3500 Rand (£150 /$215). The clinic that serves the area provides free health services and medication.
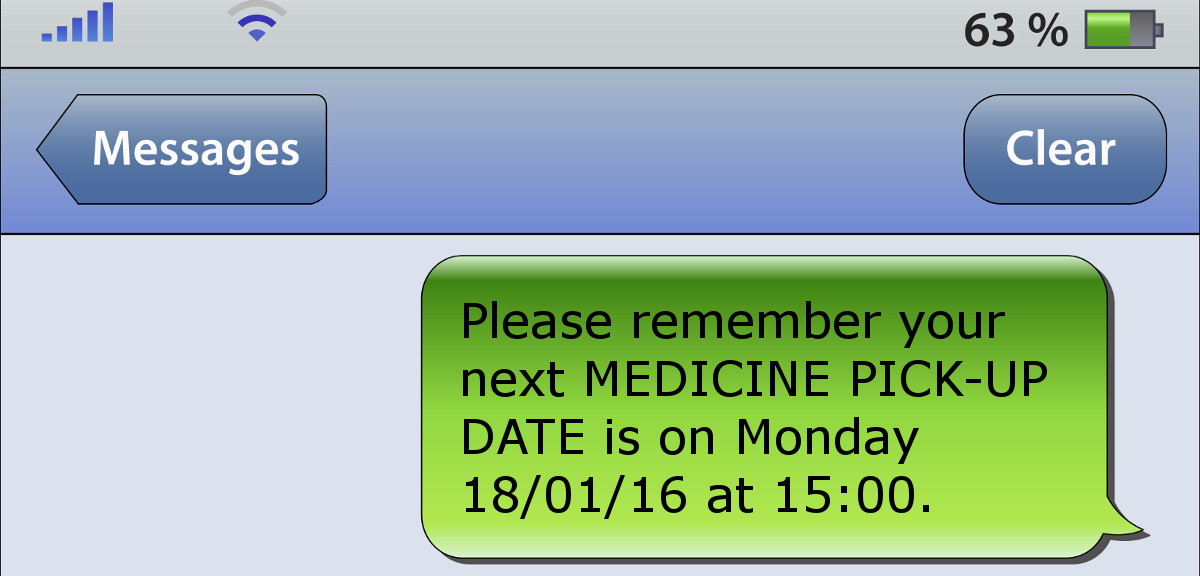
Patients were randomly split into three equal-sized groups. All patients received written information about high blood pressure and healthy living. The first group then received weekly messages at a time and in the language they chose (Afrikaans, English, or isiXhosa). The messages, designed in consultation with people in low-income communities in the area, encouraged patients to collect and take their medication and educated them about hypertension and its treatment. Extra messages were sent to remind people when medicine was ready for collection or when they had a clinic appointment.
The second group received the same text messages but were able to interact with the automated service by calling to change or cancel appointments or change the language or time of the messages. The third group received standard care.
Health workers used mobile phones linked to blood pressure measuring devices to collect health information about patients, and text messaging was managed automatically using an affordable system developed by Oxford's Institute of Biomedical Engineering.
After twelve months, all three groups had reduced blood pressure. However, those who had received text messages had a slightly greater reduction in their blood pressure and were more likely to have achieved a controlled blood pressure. Those who had had reminders were also more likely to have taken their medicine at least 80% of the time – almost two thirds of those getting information messages reached that standard compared to just under half of those receiving standard care.
Professor Farmer said: 'The improvements seen were equivalent to those expected from intensive one-to-one behavioural counselling, which is usually more expensive. When we consider that those good at sticking to treatment are 20% less likely to die prematurely than those who don’t manage that, any relatively low-cost intervention that helps people manage their high blood pressure successfully can save the very real personal, social and economic costs of the disease.'
Professor Lionel Tarassenko from Oxford's Institute of Biomedical Engineering said 'There is a great potential for mobile phone technology to help with the management of chronic diseases world-wide through automated messaging to the right person at the right time. With this study, we have demonstrated how this could be done in an area where large numbers of people are at risk because of uncontrolled blood pressure.'
The Oxford team say that further research into the optimum frequency and content of messages, and the costs of operation, are now needed.
In a linked editorial for Circulation, Julie C. Lauffenburger and Niteesh K. Choudhry, from Harvard Medical School say the study is an important scientific contribution and demonstrates the ability to conduct trials of mobile technology with rigour. They add: 'The investigators should also be commended for their use of pragmatic methods (including limited inclusion and exclusion criteria and relatively simple methods for outcome assessment) and design techniques (such as minimization) that are state-of-the-art for more traditional efficacy trials. Perhaps most importantly, the trial was also conducted in a resource-poor setting in which less evidence is available than in higher income countries.'
This trial is supported by the Oxford Centre of Excellence in Medical Engineering funded by the Wellcome Trust and the Engineering and Physical Sciences Research Council.