Oxford University researchers have found the Achilles heel of certain cancer cells – mutations in a gene called SETD2. Their findings will be presented to the National Cancer Research Institute conference in Liverpool on Monday 2 November 2015.
Oxford University researchers have found the Achilles heel of certain cancer cells – mutations in a gene called SETD2. Their findings will be presented to the National Cancer Research Institute conference in Liverpool this Monday (2 Nov 15).
It is well known that mutations drive cancer cell growth and resistance to treatment. However, these mutations can also become a weak point for a tumour. The Oxford team found that that was the case for cancer cells with mutations in a key cancer gene called SETD2.
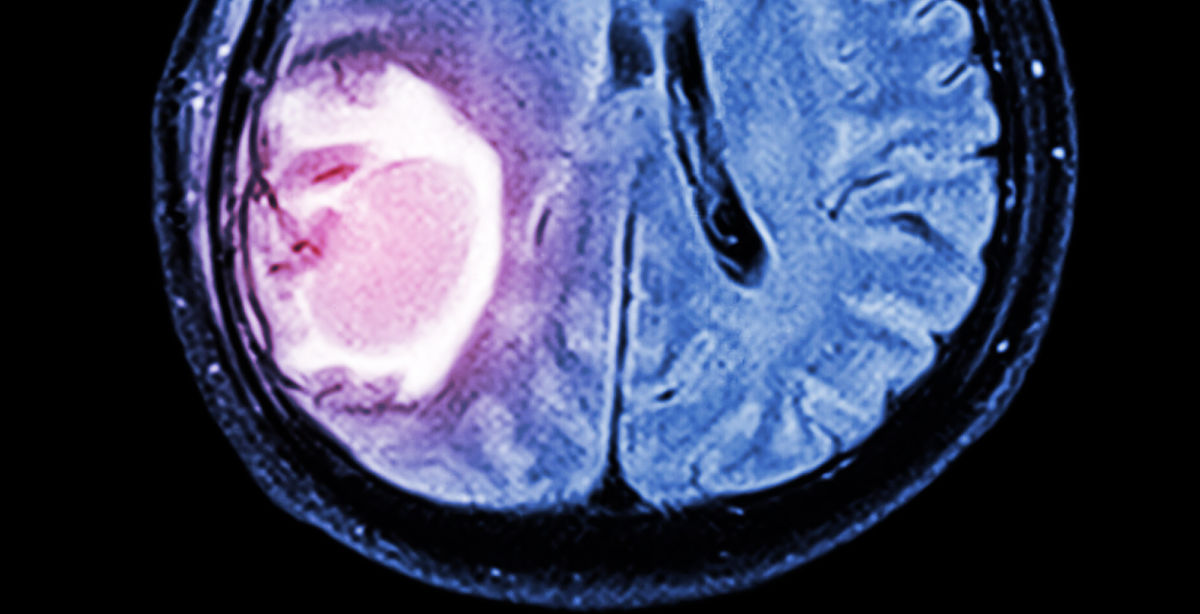
Each year around 10,000 people in the UK are diagnosed with kidney cancer, with around 54% surviving for at least 5 years. Around 9,400 people in the UK are diagnosed each year with brain and other central nervous system or intracranial tumours each year. 30% of brain tumours in children are gliomas. For high grade gliomas in both children and adults the outlook is poor.
Study author, Dr Timothy Humphrey said: 'Mutations in SETD2 are frequently found in kidney cancer and some childhood brain tumours, so we were excited when we discovered that a new drug we were studying specifically killed cancer cells with this mutation.'
The presentation will discuss how Dr Humphrey and his team showed that cancer cells with a mutated SETD2 gene were killed by a drug called AZD1775 that inhibits a protein called WEE1. WEE1 was first discovered by British Nobel Prize winner Sir Paul Nurse.
The team achieved this by exploiting the concept of 'synthetic lethality', where a combination of two factors kills a cancer cell. This has the potential to be a less toxic and more effective treatment than more standard approaches because it can specifically target cancer cells.
Synthetic lethality exploits a situation in which two pathways function together to perform an essential cellular function (in this case, both SETD2 and WEE1 control deoxynucleotide levels in the cell). If either pathway is disrupted alone, either by a drug (such as AZD1775) or a mutation (such as SETD2), cells are still viable. However, if both pathways are disrupted together (such as inhibiting WEE1 in a cancer cell with mutated SETD2), the cells die.
Co-author Dr Andy Ryan said: 'When WEE1 was inhibited in cells with a SETD2 mutation, the levels of deoxynucleotides, the components that make DNA, dropped below the critical level needed for replication. Starved of these building blocks, the cells die. Importantly, normal cells in the body do not have SETD2 mutations, so these effects of WEE1 inhibition are potentially very selective to cancer cells.'
Importantly, the research team, funded by Cancer Research UK and the Medical Research Council, have also developed a biomarker test to identify SETD2 mutated tumours, something that can be used immediately in cancer diagnosis.
Professor Tim Maughan, Clinical Director of the Cancer Research UK/Medical Research Council Oxford Institute for Radiation Oncology, said: 'This novel and exciting finding provides a new scientific basis for precision targeting of some cancers which are currently very difficult to treat, and we are now taking these findings into clinical trials.'
While there is still work to do before a treatment is available, the hope is that these findings will help to target other cancers with similar weak points and provide a step towards personalized cancer therapy.